INTRODUCTION
Have you ever searched for a recipe online and found something weird? Internet has alot of information almost about all topics. But sometimes unrealistic health myths hit your mind. “Blue Waffle.” Is such an unrealistic myth persisting on internet for years. Surprisingly majority of women are still confused if blue waffle real? In simple and straightforward words, everything you have read about blue waffle skin disease is untrue, even the fictitious pictures.
Is it true that a sexually transmitted infection can turn your private parts blue? Topics related to sexual health such as blue waffle need to be addressed through reliable resources. Never go for any unofficial and unreliable resource if it’s a concern of your health.
This blog post uncovers; where the blue waffle myth came from?, what are STIs in simple terms? , and give you trustworthy sources for sexual health information.
This blog post will make your vision crystal clear about this freaking myth of blue waffle. After reading this blog post you will be able to make others aware of STIs and the difference between the myth and reality.
What is the blue waffle?
(Spoiler Alert: It’s Not Real)
“Blue Waffle” is a hoax, a fabricated STI that has been circulating online for over a decade. “Waffle” is a slang term used for vagina.
Blue Waffle is described as turning the genitals a disturbing shade of blue, along with unpleasant symptoms. good news? None of this is true. Blue Waffle Disease is a fictional concept that has no link to sexually transmitted infections (STIs). STIs possess their own set of symptoms, which will be discussed in a later section.


Anchor: In 2018, the Centers for Disease Control and Prevention (CDC) documented 26 million new infections. Nearly half of these infections were reported among young people aged 15–24 years, according to the organizations records.
It is important to note that blue waffle disease is entirely fabricated and does not exist in the medical world. The symptoms associated with blue waffles are not real. Any image or piece of information related to this condition is false and misleading. Bad news? This myth can cause unnecessary panic and underscore the importance of reliable sexual health information.
Where Did the Wild Blue Waffle Tale Come From?
The origins of the Blue Waffle Hoax is difficult to catch. It is believed to have emerged in the late 2000s as a “bait and switch” tactic. The bait? Picture of a delicious-looking blue waffle. Switch? Clicking on the image leads to a graphic image showing the effects of the imaginary disease. All images related to the blue waffle vagina are photoshopped.
Anchor: A 2018 study showed that false rumors reach more people than the truth. They spread like fire.
Only women with numerous sexual partners were suffering from this made-up blue waffle illness. None of the pictures spreading this myth showed a picture of male genitalia. This annoying myth might be directed to tease women only!
Anchor: According to studies, none of the sexually transmitted infections (STIs) can turn your vagina blue. Blue vagina is not a symptom related to any STIs.
Why Does the Blue Waffle Myth Persist?
Internet is a very vast space and sometimes strange too. Misinformation can spread like wildfire, especially when it comes to sensitive topics like sexual health. Trendzguruji.me health and beauty tips is a reliable source that provides satisfactory information about health and beauty related topics.
Here are some possible reasons why the freaking myth of the blue waffle has stuck:
- Lack of comprehensive sex education: Lack of sexual information to the teenagers at school level is an emerging cause of persistence of such fictuous myths.
- Shock factor: Unfortunately, shock tactics can grab attention and keep the myth alive.
- Humor (of the questionable kind): Some people might spread the blue waffle hoax as a prank. While it might seem funny in the moment, it can contribute to the spread of misinformation.
So, what are real STIs like?
While the blue waffle is pure fiction, there are real STIs that can cause some pretty unpleasant symptoms. Here’s a quick brief of some common ones:
- Chlamydia
- Gonorrhea
- Trichomoniasis
- Human Papillomavirus (HPV)
Chlamydia
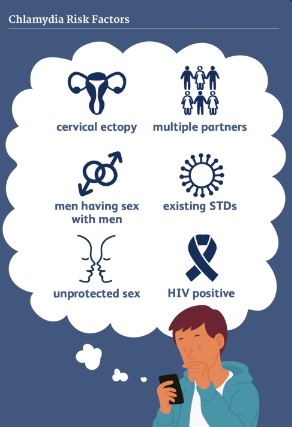
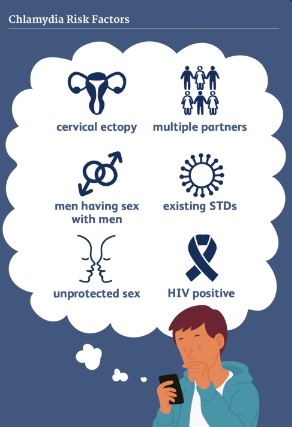
While the blue waffle is a figment of the internet’s imagination, there are real STIs with very real consequences. One such STI is chlamydia.
Chlamydia is a common bacterial infection that can affect both men and women. Unlike the outlandish claims of the blue waffle, chlamydia often goes unnoticed. This makes it even more important to be aware of its symptoms and transmission methods.
Chlamydia: The Silent STI
Chlamydia is the most frequently reported bacterial STI among young adults in the United States. The scary part? It often shows no symptoms at all. This means people can be infected without even knowing it. Unknowingly passing it on to their partners.
Anchor: Approximately one million STIs (sexually transmitted infections) are contracted globally each day, with the majority showing no symptoms.
But if there are no symptoms, how do I know if I have Chlamydia?
Regular testing is crucial for catching chlamydia early. Here’s what you need to know:
- Symptoms to Watch Out For: Though it’s uncommon but there are some potential symptoms of chlamydia include a burning sensation during urination, unusual discharge, and pelvic pain.
- Getting Tested: If you’re sexually active with new partners, getting tested for STIs is an essential part of responsible sexual health. Talk to your doctor about the best testing options for you.
The Good News? Chlamydia is Treatable!
Contrary to the mythical blue waffle, chlamydia is easily cured with a simple course of antibiotics. Early detection and treatment are key to preventing complications like pelvic inflammatory disease (PID) in women and infertility in both men and women.
By staying informed and practicing safe sex, you can navigate the world of sexual health with confidence.
Remember, the blue waffle may be a myth, but STIs like chlamydia are real. The good news? With knowledge and action, you can protect yourself and your partner.
Gonorrhea
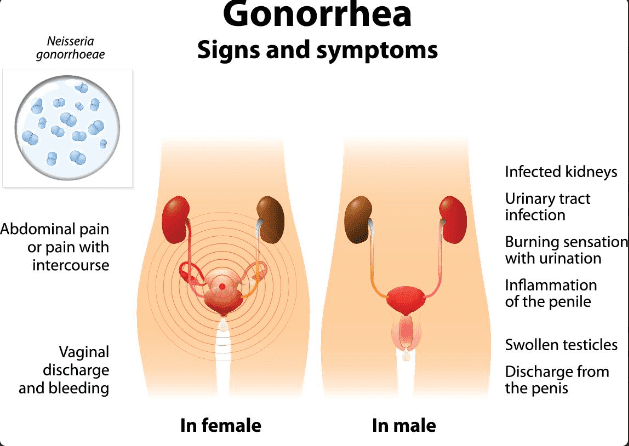
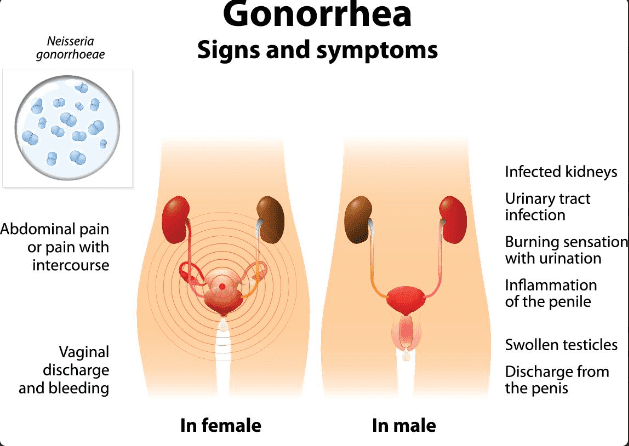
We’ve delved deep into the myth of the blue waffle and explored the realities of chlamydia. But the journey through the landscape of STIs continues. Today, we turn our attention to gonorrhea, another common bacterial infection with significant health implications.
Gonorrhea: Not a Myth, But Treatable
Unlike the blue waffle’s fabricated horrors, gonorrhea is a very real STI that can cause serious health problems if left untreated. It’s important to distinguish between the two: one is a product of internet trickery, and the other is a genuine concern for sexual health. Sperm Cramps A Myth?
Symptoms and Transmission:
Gonorrhea, like chlamydia, can sometimes be asymptomatic, particularly in women. However, when symptoms do appear, they can include:
- Burning sensation during urination
- Increased vaginal discharge
- Pelvic pain
- Painful or swollen testicles (in men)
Gonorrhea is spread through unprotected vaginal, oral, or anal sex with someone infected with the bacteria.
Early Detection and Treatment are key.
Similar to chlamydia, early detection and treatment are crucial for preventing complications from gonorrhea. If left untreated, gonorrhea can lead to pelvic inflammatory disease (PID) in women, ectopic pregnancy, and even infertility in both men and women.
Anchor: STIs can raise the risk of HIV and have a direct impact on sexual and reproductive health through stigmatization, infertility, cancer, and pregnancy complications.
The Power of Antibiotics:
The good news? Just like chlamydia, gonorrhea is curable with a course of antibiotics. However, it’s important to complete the entire prescribed medication regimen to ensure complete eradication of the bacteria.


Trichomoniasis
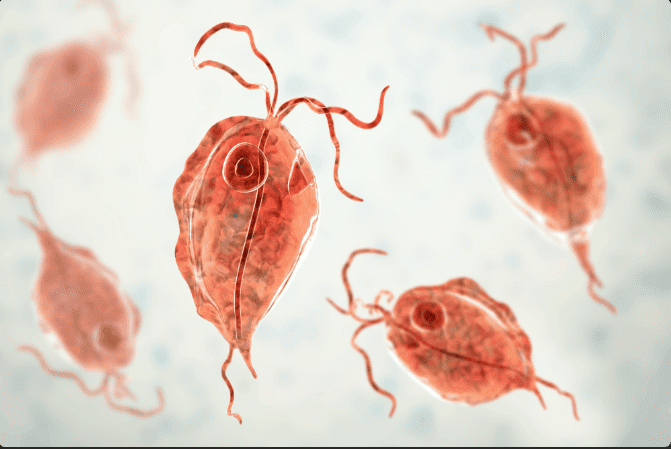
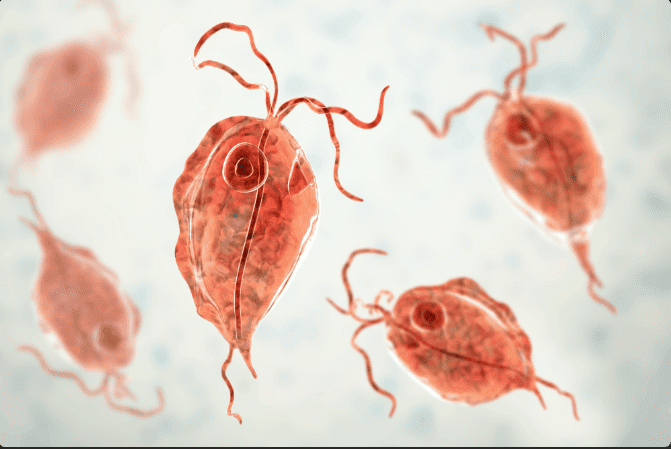
We’ve delved into the myth of the blue waffle and explored the realities of chlamydia and gonorrhea. Our journey through the landscape of STIs continues with trichomoniasis, a parasite-caused infection that can cause irritation and discomfort.
Trichomoniasis: A Parasite Among Us
Unlike chlamydia and gonorrhea, which are caused by bacteria, trichomoniasis is caused by a tiny parasite called Trichomonas vaginalis. While not as well-known as its bacterial counterparts, trichomoniasis is actually a common STI, particularly among young adults.
Symptoms and Transmission:
Trichomoniasis often goes undiagnosed because many people don’t experience any symptoms at all. However, when symptoms do occur, they can include:
- Vaginal itching and burning
- Painful urination
- Increased vaginal discharge with an unpleasant odor
Trichomoniasis is spread through vaginal, oral, or anal sex with someone infected with the parasite. It’s important to note that unlike some other STIs, trichomoniasis can survive for a short time outside the body in moist environments.
Treatment and Preventing Complications:
Thankfully, trichomoniasis is curable with a single dose of antibiotics or a short course of medication. However, it’s important to treat both sexual partners to prevent re-infection. Left untreated, trichomoniasis can increase the risk of contracting other STIs, including HIV.
Human Papilloma Virus HPV
Our exploration of STIs continues with a shift from the realm of bacteria and parasites to the world of viruses. Today, we tackle the human papillomavirus (HPV), a very common virus with diverse implications for sexual health.
HPV: More Than Just Warts
Unlike the blue waffle’s fabricated horrors, HPV is a real virus that can cause a variety of health problems, including genital warts and certain types of cancer. However, it’s important to understand that not all HPV strains are created equal.
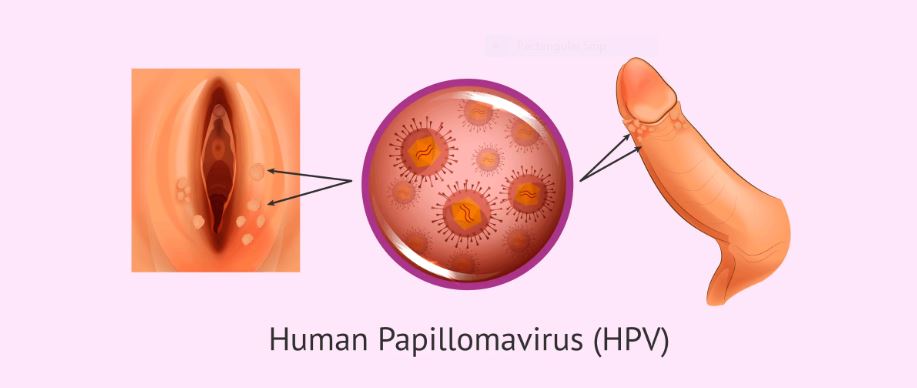
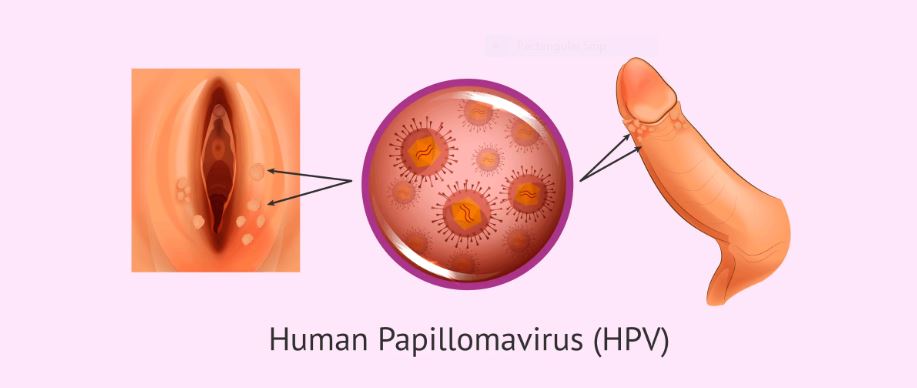
The Spectrum of HPV:
There are over 150 different strains of HPV, and most people will come into contact with at least one type in their lifetime. Here’s a breakdown of the different types:
- Low-Risk HPV: These strains are responsible for causing genital warts, which are noncancerous growths on the genitals or anus. While not life-threatening, they can be bothersome and require treatment.
- High-Risk HPV: Certain HPV strains are considered high-risk because they can contribute to the development of certain cancers, including cervical cancer, vaginal cancer, vulvar cancer, anal cancer, and some head and neck cancers.
The Importance of Vaccination:
The good news? There is a vaccine available that can protect against the most common strains of HPV, including both low-risk and some high-risk types. Vaccination is most effective when administered to preteens (ages 11–12), but it can be given up to age 45 for those who haven’t been vaccinated yet.
Early Detection and Treatment:
Regular Pap smears and HPV testing are crucial for the early detection of cervical cancer and precancerous lesions. Early detection allows for timely intervention and treatment, significantly improving the prognosis.
Living with HPV:
Even if you’ve been diagnosed with HPV, it doesn’t mean you’ll automatically develop cancer. Most HPV infections clear up on their own within a few years. However, regular screening remains essential for monitoring your health.
Essential Steps in STI Prevention
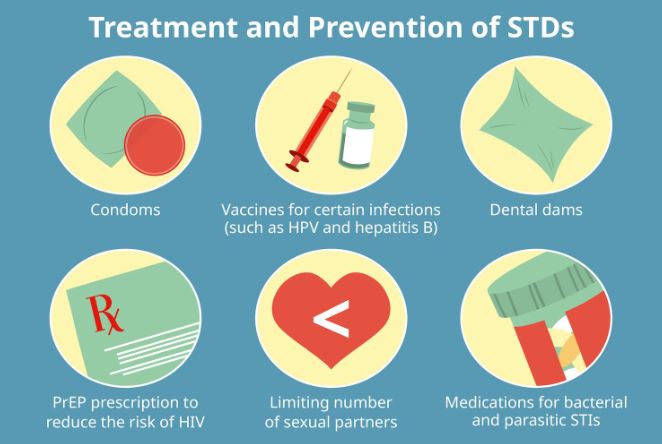
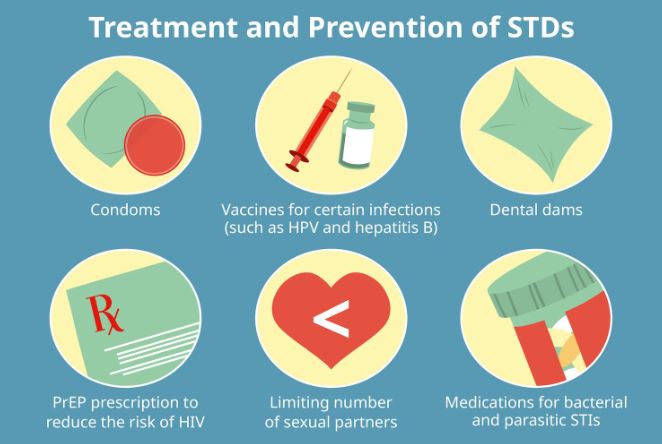
We have explored the realities of various STIs and waded through the murky waters of the blue waffle myth. Now, let’s shift gears and equip you with a powerful arsenal of strategies for preventing STIs in the first place.
Knowledge is Power:
The first step in STI prevention is arming yourself with knowledge. Here are some key things to understand:
- Types of STIs: Familiarize yourself with the most common STIs, their symptoms, and their potential consequences.
- Transmission Methods: Learn how STIs are spread through various forms of sexual contact.
- Testing Options: Understand the different testing methods available for STIs and their frequency based on your sexual activity.
Embrace Safe Sex Practices:
The cornerstone of STI prevention lies in practicing safe sex. Here are some essential steps:
- Condom Consistency: Consistently and correctly use condoms during vaginal, anal, and oral sex.
- Beyond Latex: If you have a latex allergy, explore alternative condom options like polyurethane.
- Dental Dams for Oral Sex: Use dental dams to create a barrier during oral sex and minimize risk.
Communication is Key:
Open and honest communication with your sexual partner(s) is crucial for responsible sexual health:
- STI History Disclosure: Consider disclosing your STI history and discussing your partner’s status before engaging in sexual activity.
- Respecting Boundaries: Respect your partner’s boundaries and expectations regarding sexual activity.
- Negotiating Safe Sex Practices: Openly discuss and agree upon safe sex practices with your partner(s) before intimacy begins.
Embrace Regular Testing:
Regular testing for STIs is an essential component of responsible sexual health:
- Testing Frequency: Discuss with your doctor how often you should be tested for STIs based on your sexual activity level and risk factors.
- Early Detection, Early Treatment: Early detection of STIs allows for prompt treatment and minimizes the risk of complications.
- Partner Notification: If you are diagnosed with an STI, it’s important to notify your partner(s) so they can get tested and treated as well.
Building a Healthy Sexual Future:
By following these essential steps, you can significantly reduce your risk of contracting an STI and protect your sexual health. Remember, safe sex practices not only safeguard you but also promote the well-being of your partner(s).
Shattering the Silence: Addressing Shame and Stigma Around STIs
We’ve thoroughly debunked the blue waffle myth and delved into the realities of STIs, equipping you with knowledge and preventative measures. Now, let’s address a critical yet often overlooked aspect of sexual health – shame and stigma surrounding STIs.
The Shadow of Stigma:
Unfortunately, STIs are often shrouded in shame and secrecy. This can deter people from getting tested, seeking treatment, or talking openly about their sexual health. Here’s why dismantling the stigma is crucial:
- Delayed Diagnosis: Fear of judgment can lead to delayed testing, potentially allowing an STI to progress and cause complications.
- Untreated STIs: Untreated STIs can have serious health consequences, including infertility and an increased risk of certain cancers.
- Perpetuating the Cycle: The stigma fuels misinformation and discourages open communication, hindering efforts to prevent the spread of STIs.
Breaking the Cycle:
Here’s how we can all contribute to dismantling the stigma surrounding STIs:
- Open Communication: Normalize talking about sexual health with friends, partners, and healthcare providers.
- Challenge Misconceptions: Educate yourself and others about STIs, dispel myths, and promote accurate information.
- Empathy and Support: Show compassion and understanding towards people living with STIs. Remember, STIs are treatable and not a moral failing.
- Embrace Advocacy: Support organizations working towards sexual health education and STI awareness campaigns.
Remember, You’re Not Alone:
STIs are incredibly common. In fact, millions of people around the world live with them. If you have an STI, it doesn’t define you. There are effective treatments available, and a supportive community exists to help you navigate your health journey.
Taking Charge of Your Sexual Health
By acknowledging the stigma and taking steps to dismantle it, we can create a space for open communication and responsible sexual health practices. The next section will provide valuable resources for further information, testing options, and support services for those living with STIs.
STI Testing


We’ve embarked on a journey that shattered the blue waffle myth, explored the realities of STIs, and unpacked the weight of stigma. Now, let’s delve into the practical side of things: getting tested for STIs.
Why Get Tested?
STI testing is a crucial component of responsible sexual health. Here’s why regular testing is important:
- Early Detection: Early diagnosis allows for prompt treatment, minimizing the risk of complications and transmission to partners.
- Peace of Mind: Getting tested and knowing your status can provide peace of mind and allow you to make informed decisions about your sexual health.
- Protecting Your Partner(s): By getting tested, you’re taking an active role in protecting your partner(s) from STIs.
Where to Get Tested?
There are a variety of options available for STI testing, including:
- Doctor’s Office: Schedule an appointment with your doctor for a comprehensive STI screening.
- Planned Parenthood: Planned Parenthood centers offer affordable and confidential STI testing.
- Public Health Clinics: Many public health clinics offer free or low-cost STI testing.
- At-Home Tests: Home test kits for certain STIs are available over-the-counter, but confirmation testing by a healthcare professional is usually recommended.
What to Expect During a Test?
The specific type of test you receive will depend on the STI being tested for. Here’s a general overview:
- Urine Sample: This is a common method for testing for chlamydia, gonorrhea, and trichomoniasis.
- Swab Test: A swab is used to collect a sample of cells from the vagina, cervix, penis, or rectum for testing for various STIs.
- Blood Test: Blood draws can be used to test for certain STIs, like HIV and syphilis.
Confidentiality and Support:
STI testing is confidential. Healthcare providers are legally bound to protect your privacy. Many testing centers offer support services and can answer any questions you might have.
Moving Forward After Testing:
If your test results are positive, don’t panic. There are effective treatments available for most STIs. Your healthcare provider will discuss the best course of action for you and your partner(s).
Remember:
- Early detection and treatment are key for optimal outcomes.
- There is no shame in having an STI.
- You are not alone. Many people live with STIs, and support services are available.
Frequently Asked Questions
Can you get blue waffle “symptoms” from frequent sex?
No, you absolutely cannot get “blue waffle symptoms” from frequent sex. The “blue waffle” is a completely fabricated internet hoax. It’s not a real sexually transmitted infection (STI) and the graphic imagery associated with it is entirely fictional.
Frequent sex can sometimes lead to irritation or discomfort in the genital area, but these symptoms are usually mild and temporary. If you experience any persistent discomfort after sex, it’s best to consult a healthcare professional to rule out any underlying conditions.
What are the symptoms of blue waffle?
The good news (or maybe strange news) is that you won’t experience any symptoms of the “blue waffle” because it’s entirely fictional. It’s an internet hoax designed to shock and mislead people about sexual health. There’s no STI that causes the genitals to turn blue, nor any of the other graphic symptoms associated with the myth.
However, if you’re concerned about potential symptoms related to frequent sex or sexual activity, here are some things to keep in mind:
- Irritation: Frequent sex can sometimes lead to mild irritation in the genital area, especially if you’re not using lubrication. This can manifest as redness, itching, or a burning sensation.
- Yeast Infection: If the irritation is accompanied by a thick, white discharge and burning during urination, it could be a yeast infection. This is a common fungal infection that’s easily treated with medication.
- Bacterial Vaginosis: Another possibility is bacterial vaginosis (BV), which can cause a thin, grayish discharge with a fishy odor. While not an STI, BV can occur after sex due to changes in vaginal flora.
Remember:
- If you experience any persistent discomfort after sex, it’s always best to consult a healthcare professional. They can diagnose the cause and recommend the appropriate treatment.
How long does blue waffle last?
The “blue waffle” doesn’t actually exist, so it doesn’t have a duration. It’s a completely fabricated internet myth with no basis in reality. There’s no STI that causes the symptoms often associated with the hoax.
Here’s a quick recap:
- Blue waffle is fake: It’s an internet prank designed to mislead people about sexual health.
- No blue symptoms: There are no real STIs that cause the graphic symptoms associated with the myth.
- Focus on real concerns: If you’re experiencing any discomfort after sex, consult a healthcare professional. They can diagnose the cause and recommend treatment.
Why Sex Education Is Important?
Sex education goes far beyond the mechanics of reproduction. It’s a crucial component of a healthy upbringing, equipping young people with the knowledge, skills, and confidence to navigate the complexities of their sexuality. Here’s why sex education deserves a prominent place in our educational systems:
- Combating Ignorance and Misinformation: The internet is a breeding ground for misinformation, and sex is no exception. Comprehensive sex education combats myths and misconceptions with accurate information, empowering young people to make informed decisions about their sexual health.
- Promoting Healthy Relationships: Sex education goes beyond just physical intimacy. It teaches essential skills for building healthy relationships, including communication, consent, and respect for boundaries. These skills are invaluable not just for romantic relationships but for all aspects of life.
- Preventing STIs and Unplanned Pregnancy: Knowledge is power, especially when it comes to sexual health. Sex education equips young people with the knowledge about sexually transmitted infections (STIs) and methods of contraception. This knowledge can significantly reduce the risk of unplanned pregnancies and infections.
- Building Self-Esteem and Body Positivity: Sex education creates a space for open discussions about body image and self-acceptance. It can help young people develop a positive and healthy relationship with their bodies.
- Identifying and Preventing Abuse: Many sex education programs incorporate lessons on recognizing and preventing sexual abuse. This empowers young people to protect themselves and seek help if needed.
Benefits Beyond the Individual:
The positive effects of sex education extend beyond the individual:
- Reduced Healthcare Costs: By preventing STIs and unplanned pregnancies, comprehensive sex education can significantly reduce healthcare costs for individuals and society as a whole.
- Safer Communities: When young people understand consent and healthy relationships, it contributes to safer communities with less sexual violence.
Who needs STI testing?
Generally, anyone who is sexually active should get tested for STIs at some point. Here are some specific situations where testing is especially recommended:
- People with new sexual partners: It’s crucial to get tested before starting a new sexual relationship, especially if you or your partner(s) have had multiple partners in the past.
- People in ongoing relationships: Even in committed relationships, regular testing is important. This is because some STIs can be asymptomatic, meaning you might not experience any symptoms even if you’re infected.
- People who have had unprotected sex: Unprotected sex, meaning sex without a condom or other barrier method, significantly increases the risk of contracting an STI. Getting tested after unprotected sex is essential.
- People who experience STI symptoms: Symptoms like burning during urination, unusual discharge, pelvic pain, or genital warts can be signs of an STI. Getting tested is crucial to determine the cause and receive prompt treatment.
- Pregnant women: Certain STIs can be passed from mother to baby during pregnancy. Pregnant women should be tested for specific STIs as part of their prenatal care.
Here are some additional factors to consider:
- Age: Young adults (ages 15-24) are at a higher risk for contracting STIs.
- Number of sexual partners: The more sexual partners you have, the greater your risk of contracting an STI.
- History of STIs: If you’ve had an STI in the past, you’re at a higher risk of contracting another one.
Ultimately, the decision of whether or not to get tested for STIs is a personal one. However, by understanding the risk factors and the benefits of testing, you can make an informed choice about your sexual health.
What to tell your doctor before an STI test?
Here’s what you should tell your doctor before an STI test to ensure a smooth and informative experience:
Your Sexual History:
- Number of Sexual Partners: Be honest about the number of sexual partners you’ve had recently (past few months) and in the past year.
- Types of Sexual Activity: Inform your doctor about the types of sexual activity you engage in (vaginal, anal, oral) to determine the most appropriate testing methods.
- Condom Use: Let your doctor know if you consistently use condoms or other barrier methods.
- New or Multiple Partners: Mention if you have a new sexual partner or multiple partners, as this can influence the testing approach.
Symptoms (if any):
- Describe any symptoms you’ve been experiencing, including:
- Burning sensation during urination
- Unusual discharge (color, consistency, odor)
- Pelvic pain
- Genital warts or sores
Past STIs:
- Disclose if you’ve ever been diagnosed with an STI in the past.
- Mention any past treatments you received.
Medications:
- Inform your doctor about any medications you’re currently taking, as some medications can interact with STI testing.
Additional Concerns:
- Pregnancy: Let your doctor know if you’re pregnant or planning to become pregnant, as this may influence the types of tests used.
- Partner Notification: Ask your doctor about partner notification services, which can help notify your sexual partner(s) about the need for testing and treatment.
Open Communication is Key:
Don’t hesitate to ask your doctor any questions you may have about STIs, testing procedures, or treatment options. The more information you share, the better equipped your doctor is to provide you with personalized care and guidance.
Remember:
- There’s no shame in getting tested for STIs.
- It’s a responsible way to protect your sexual health and the health of your partner(s).
- Your doctor is there to help – they’ve likely seen and heard it all before.
What types of STI tests are there?
There are various types of STI tests available, depending on the specific STI being checked for. Here’s a breakdown of some common testing methods:
Urine Tests:
- This is a convenient and non-invasive method used to test for chlamydia, gonorrhea, and sometimes trichomoniasis. A urine sample is collected in a cup and sent to a lab for analysis.
Swab Tests:
- Swab tests involve gently collecting a sample of cells from the cervix, vagina, urethra, or rectum using a cotton swab. These swabs are then tested for various STIs, including:
- Chlamydia
- Gonorrhea
- Trichomoniasis
- HPV (human papillomavirus) in some cases
- Herpes (depending on the type and if there’s a visible sore)
Blood Tests:
- Blood draws are used to detect certain STIs like:
- HIV
- Syphilis
- Hepatitis B and C
Other Tests:
- Lumbar puncture (spinal tap): This is a more invasive procedure used in rare cases to diagnose advanced stages of syphilis or certain neurological complications from STIs.
Rapid Tests:
- Some clinics offer rapid tests for certain STIs, such as HIV and chlamydia. These tests provide results within a short timeframe, sometimes in as little as 10-30 minutes. However, they may not be as sensitive as traditional laboratory tests, and confirmatory testing might be recommended.
At-Home Tests:
- Over-the-counter home test kits are available for some STIs, like chlamydia and trichomoniasis. These tests can offer a convenient option; however, confirmatory testing by a healthcare professional is usually recommended for accuracy.
The Right Test for You:
The type of STI test your doctor recommends will depend on several factors, including:
- Your symptoms (if any)
- Your sexual history
- The specific STI(s) you’re concerned about
Summary
The “blue waffle” is a complete hoax. It’s not a real STI and the graphic imagery associated with it is entirely fictional. There’s no need to worry about experiencing any symptoms related to it. Focus on real sexual health practices and don’t hesitate to seek accurate information from trusted sources.
REFERENCES
- Planned Parenthood: Planned Parenthood: https://www.plannedparenthood.org/
- Centers for Disease Control and Prevention (CDC): CDC – Sexually Transmitted Diseases: https://www.cdc.gov/std/default.htm
- National Sexual Health Resource Center: National Sexual Health Resource Center: https://www.plannedparenthood.org/get-care/our-services
- American Sexual Health Association: American Sexual Health Association: https://www.ashasexualhealth.org/
- National Institutes of Health (NIH): https://www.ncbi.nlm.nih.gov/books/NBK573163/


[…] consulting with a healthcare specialist is advisable for a proper diagnosis and tailored treatment. Blue Waffle a myth! 1. Infection: Infections, such as epididymitis or prostatitis, can induce sperm cramps by […]